
Migraines
Natural Solutions for Chronic Migraines & Headaches
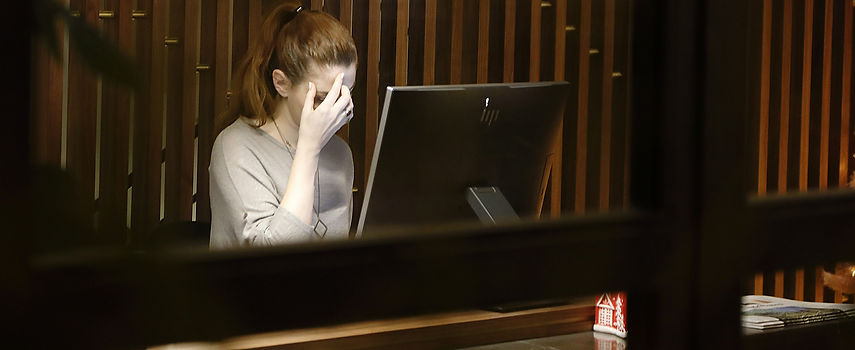
Migraines are not “just headaches.” They are complex neurological events that can disrupt your work, relationships, sleep, digestion, and quality of life. For many people, migraines come with nausea, light and sound sensitivity, visual changes, brain fog, and a lingering sense of exhaustion long after the pain fades.
If you’ve been told migraines are something you simply have to manage with medication, avoid triggers, or “live with,” you’re not alone. But migraines rarely occur without an underlying reason.
As a Naturopathic Doctor, I help patients understand why their migraines are happening by identifying the root causes of contributing to migraine attacks.
What Causes Migraines?
Migraines develop when the nervous system becomes overly sensitive and reactive. This sensitivity is often driven by a combination of internal stressors that affect inflammation, blood vessel regulation, neurotransmitters, hormones, and gut-brain communication.
Common contributors include:
-
Gut microbiome imbalances and digestive dysfunction
-
Food sensitivities and immune activation
-
Hormonal fluctuations
-
Chronic stress and nervous system dysregulation
-
Inflammation
-
Blood sugar instability
-
Nutrient deficiencies
Rather than searching for a single trigger, effective migraine care looks at the patterns that overload the nervous system over time.
Common Root Causes of Migraines
The Gut–Brain Connection & Migraines
The gut and brain are in constant communication through the gut-brain axis. The gut microbiome plays a critical role in regulating inflammation, neurotransmitter production (including serotonin), immune function, and the stress response.
Imbalances in the gut microbiome, intestinal permeability (also known as “leaky gut”), or poor digestion can increase systemic inflammation and trigger immune responses that sensitize the nervous system.
Many migraine patients also experience:
-
IBS, constipation, diarrhea, or chronic bloating
-
Food reactions that seem inconsistent or unpredictable
-
Nausea or appetite changes around migraines
Supporting gut health is a key step in reducing migraine frequency and intensity.
Food Sensitivities & Immune Activation
Food sensitivities do not always cause immediate symptoms. In some cases, they create delayed immune responses that increase inflammation and nervous system reactivity hours or even days later.
When the gut barrier is compromised, partially digested food particles can enter circulation and stimulate immune activity, contributing to migraines, pain, fatigue, and brain fog.
Identifying and addressing food-related immune triggers can help reduce the overall inflammatory load on the body and decrease the frequency and intensity of migraines.
Hormones & Migraines
Hormonal fluctuations are a common and often overlooked migraine trigger.
Changes in estrogen, progesterone, cortisol, and blood sugar levels can influence:
-
Blood vessel dilation and constriction
-
Neurotransmitter balance
-
Pain sensitivity
-
Inflammatory signaling
This is why many patients experience migraines correlating to their menstrual cycle, during perimenopause or menopause, and during times of chronic stress or burnout.
Balancing hormones requires addressing stress physiology, gut health, nutrient status, and metabolic stability, not just hormone levels alone.
Stress, The Nervous System & Migraine Threshold
Stress is not just emotional, it is physical too.
In people with migraines, the stress response often becomes overactive, lowering the threshold at which the nervous system triggers a migraine. This means that relatively small stressors, such as skipped meals, poor sleep, certain foods triggers, and sensory overload can trigger a migraine.
Chronic stress affects cortisol (your stress hormone) and melatonin (your sleep hormone) balance, blood sugar stability, digestive function, sleep quality, and overall inflammation.
Reducing migraine attacks often requires both removing physical stressors (such as inflammation, nutrient deficiencies, inflammatory foods, and digestive dysfunction), as well as reducing mental emotional stress.
My Root-Cause Approach to Migraine Care
Migraines are highly individual. There is no single plan that works for everyone.
Your care may include:
-
A comprehensive health history and migraine pattern assessment
-
Evaluation of digestion, gut health, the gut microbiome, and food reactions
-
Targeted lab testing to assess nutrients, hormones, inflammation, immune function, and metabolic function
-
Nutrient repletion to support neurological stability
-
Supporting a healthy stress response and nervous system regulation
-
Lifestyle guidance designed to be realistic and sustainable
The goal is not to suppress symptoms, but to reduce the underlying triggers to prevent migraines from recurring.
Improvements In Your Migraines Are Possible
With the right plan, many patients notice improvements such as:
-
Fewer migraine days per month
-
Reduced intensity and shorter duration of attacks
-
Improved digestion and food tolerance
-
Better energy and sleep
-
Increased confidence in managing their health
Healing migraines is not about perfection or avoiding everything you enjoy, it’s about reducing reactivity and triggers so your nervous system is no longer on edge.
A Care Plan Built Around You
If migraines are controlling your schedule, limiting your plans, or leaving you anxious about when the next attack will hit, there may be more going on beneath the surface.
You deserve care that looks at the full picture, not just relieving the pain in your head.
